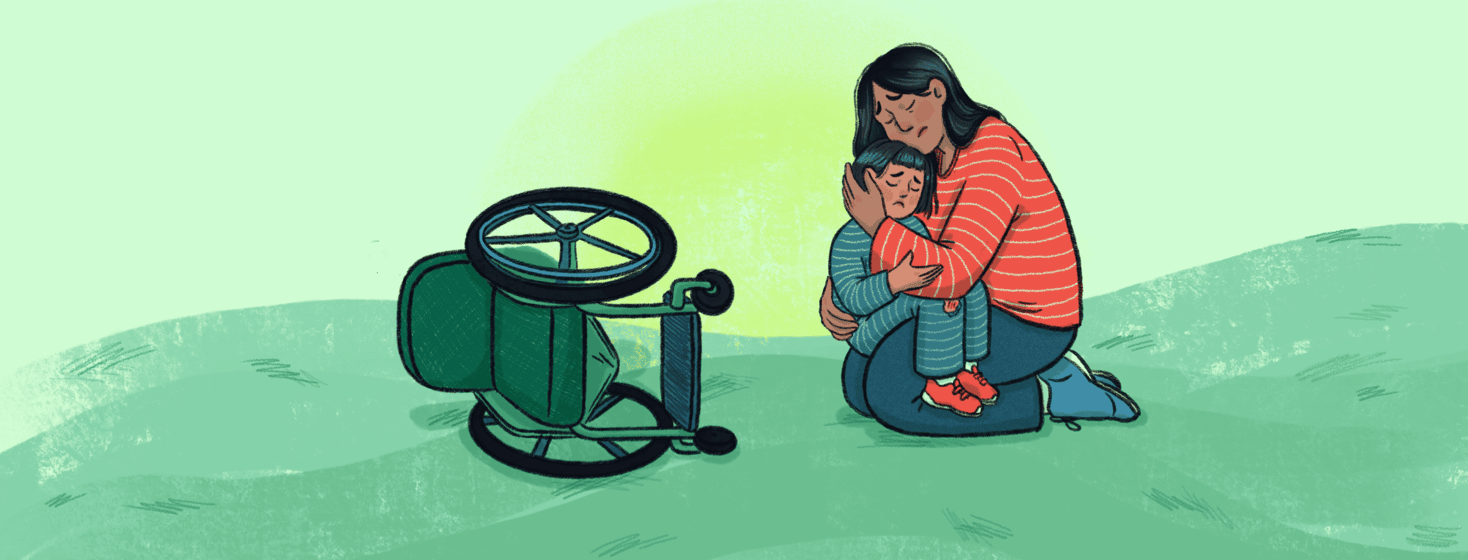
If You Fall, I’m Going Down With You
My sweet child, she’s fearless.
She’s put me at max speed.
She’s "Daddy look at me!"
She’s full of constant laughter and joy.
She's trapped in a body that won't move the way she wants it to.
And her movement, her speed…it scares me. It has scarred me.
Her first serious fall
She fell once, barely 2 years old. Pushed herself through an open door into the garage. Landed down several stairs. On the concrete. On her head. I was not far away. We didn’t know she was strong enough to go over the threshold. She didn’t know what stairs were. She had never been allowed to fall. Or able to, with her spinal muscular atrophy. The screams of her father and her own are forever in my nightmares. PTSD 1 of many. She had a skull fracture, but was ultimately okay.
We sold that house a few months later. I could barely walk through the garage.
An accident at school
She fell again, at the beginning of her kindergarten year while at recess. She was playing with a classmate. She was probably yelling faster as her friend pushed her chair. They hit a pavement edge and tipped it over. I was out of town and received the calls from the school. The response seemed too casual. I was panicked, angry and across the country. Emma was upset and said I should have been there to catch her. I never saw the film footage from the playground. Her father managed all the aftermath at home. But the learning opportunity was clear.
A tipped wheelchair is a big deal
I asked our team of experts at our children’s hospital. What is the protocol here? What is the right response. If it happened in front of me, my assessment is so immediate it’s impossible to teach. Consciousness? Positioning of her arms and neck? What did she land on? All of the things…it’s one thought…not a checklist.
And sharing the importance to her school team of why injury is so catastrophic was key in understanding the appropriate reaction. If she breaks her arm and then develops a contracture, she can then lose the ability to propel her manual wheelchair. Big deal.
Creating a response plan
A detailed plan was put in place. It was a typical Friday morning, I saw the document sent home from school, made a few changes and ferried it back to school in her backpack. Off she went on the bus, off I went to a massage.
15 mins in…my phone is lighting up. Things are bad. Her chair has flipped forward. ugh. She’s landed on her head.
The chair flips again
The PTSD response to an incident like this is pretty intense. The rush of adrenaline. The race to my car, to her, the multi-levels of evaluation and coordination that are happening simultaneously are exhausting.
Skip to the end. She’s okay. She’s totally fine. I reviewed the film in the principals office, she was self propelling, no one near her, having a blast at recess like a 5-year old does and hit a seam in the pavement. It was like watching a train wreck in slow motion. The chair slightly tipped, her feet hit the ground and then the chair proceeded to somersault over. Landing of course on her forehead, on concrete.
I don’t think the principal is accustomed to having parents swear as much as I did watching that two minute video. Angry, sick to my stomach and somehow also crying. Simply re-telling this story is making me nauseous.
Maintaining my mental balance
As parents with a delicate child whose life you are literally fighting to save on a daily basis we have all come across our moments of trauma. And they stick with us…haunting us. Its monitors beeping, ambulance sirens, codes called overhead at the hospital, bright lights at night and sweet foreheads on concrete.
We are constantly ducking out of the way of panic. I personally have had to do so much therapy, EMDR and CBT in order to not be in a fixed state of fight or flight. I go to yoga so that my brain can heal. So that my body is exhausted. I sit in the sun because my heart can be so dark all the time. I read books instead of watching tv because your brain relaxes in a different way, and you can’t actually stress at the same time.
Learning my limits
I protect my balance and I retreat when I know things are getting to a point of “too much”. I also know the bad habits I have that don’t help me - and when that “too much” point is tipping, to consciously avoid them, or ask for help.
When my daughter has a day like she did, I know that the next week is going to be awful for me. It will be hard to reset and I guarantee that I will struggle. But she gets back up. So can I.
Join the conversation